Aerodigestive Disorders
The scope of this Practice Portal page is aerodigestive disorders that affect feeding, swallowing, voice, and/or respiration in children and adults.
Structural abnormalities and complex medical conditions of the aerodigestive tract that affect feeding, swallowing, voice, and/or laryngeal airway function are also discussed to varying degrees in ASHA's Practice Portal pages on Dysphagia (Adult), Dysphagia (Pediatric) – Feeding and Swallowing, Cleft Lip and Palate, Head and Neck Cancer, Voice Disorders, and Tracheostomy and Ventilator Dependence.
Aerodigestive Tract
The aerodigestive tract consists of the organs and tissues of the respiratory tract and the upper part of the digestive tract (Andrews, 2006). The aerodigestive tract includes the
- airway (pharynx and larynx),
- pulmonary tract (trachea, bronchi, and lungs), and
- upper digestive tract (esophagus).
Breathing and swallowing functions take place in the aerodigestive tract. Both tasks elicit a complex, coordinated biomechanical sequence of events designed to protect the airway during eating and drinking, while maintaining sufficient airflow for phonation (Coyle, 2010; Jadcherla, 2012; Robbins, 2011).
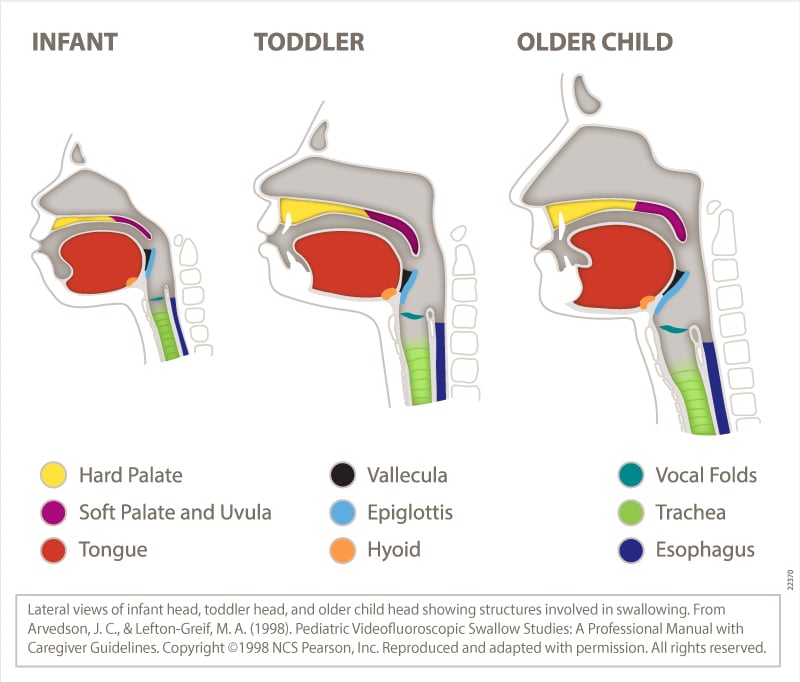
The aerodigestive anatomy and physiology of infants is different from that of adults (see figure below). These differences include the following:
- In infants, the tongue fills the oral cavity, and the velum (soft palate) is in close proximity to the epiglottis. The hyoid bone and the larynx are positioned higher in infants than in adults, and the larynx elevates less in infants than in adults during the pharyngeal phase of the swallow.
- Rapid suck–swallow sequences are characteristic of infant bottle-feeding and/or breastfeeding during sucking bursts. Precise coordination of sucking, swallowing, and respiration is essential for maintaining airway protection.
- The close proximity of oral structures and the sucking pads in the cheeks (in term infants) may provide positional stability to support efficient sucking action during bottle-feeding and breastfeeding.
- Once the infant begins eating pureed food (around 4–6 months), the oral and pharyngeal phases are similar to those of an adult (although with less elevation of the larynx).
- As the child matures, the intraoral space increases as the mandible moves downward and forward, and the oral cavity elongates in the vertical dimension. The space between the tongue and the palate increases, and the larynx and the hyoid bone descend, elongating and enlarging the pharynx (Logemann, 1998; Matsuo & Palmer, 2008).
Aerodigestive Disorders
Aerodigestive disorders are conditions or diseases of the aerodigestive tract—including the airway (pharynx and larynx), pulmonary tract (trachea, bronchi, and lungs), and upper digestive tract (esophagus)—that may affect respiratory and swallowing functions. Aerodigestive disorders, or the management of them (e.g. surgery, intubation), may result in voice, feeding, and/or swallowing problems as well as laryngeal airway problems—the term used in this Practice Portal page to refer to paradoxical vocal fold movement (PVFM) and chronic cough.
Aerodigestive disorders may be congenital, developmental, or acquired. They are not mutually exclusive—individuals may have more than one disorder (Jadcherla, 2012). In children, some aerodigestive disorders may resolve with maturity or with behavioral management, but others may require medical and/or surgical intervention.
Examples of common aerodigestive disorders (grouped by anatomical location) include, but are not limited to, the following:
Airway (Pharynx and Larynx)
- chronic cough
- dystussia
- epiglottitis
- fungal infections of the pharynx or the larynx (e.g., blastomycosis [rare], histoplasmosis, candidiasis)
- irritable larynx
- laryngeal clefts
- laryngeal or pharyngeal paralysis/paresis (unilateral or bilateral)
- laryngeal stenosis (supraglottic, glottic, or subglottic)
- laryngeal webs
- laryngomalacia (moderate to severe)
- laryngopharyngeal reflux
- laryngospasm
- muscle tension dysphagia
- muscle tension dysphonia
- PVFM
- breathing–swallowing incoordination (secondary to medical conditions such as chronic obstructive pulmonary disease (COPD), neurological insult, or head and neck cancer)
- structural or physiologic changes secondary to injury, neoplasms, radiation therapy, or surgery (e.g., pharyngeal or laryngeal resections, radiation for head and neck cancer treatment, prolonged intubation)
- velopharyngeal dysfunction
See Aerodigestive Disorders of the Airway (Pharynx and Larynx) [PDF].
Pulmonary Tract (Trachea, Bronchi, and Lungs)
- bronchomalacia
- chronic lung disease (e.g., asthma, emphysema, COPD)
- infectious diseases affecting pulmonary function (e.g., upper respiratory infection, pertussis [whooping cough], pneumonia, tuberculosis)
- neoplasms
- structural or physiologic changes affecting pulmonary function secondary to injury or surgery (e.g., pneumothorax [collapsed lung], pneumonectomy, lung transplantation)
- tracheal stenosis
- tracheoesophageal fistula
- tracheomalacia
See Aerodigestive Disorders of the Pulmonary Tract (Trachea, Bronchi, and Lungs) [PDF].
Upper Digestive Tract (Esophagus)
- esophageal motility disorder, including spasm and achalasia
- esophageal structural disorder, including stricture, web, diverticulum, and ring
- gastroesophageal reflux
- inflammatory forms of esophagitis (e.g., eosinophilic, viral, reflux-related)
See Aerodigestive Disorders of the Upper Digestive Tract (Esophagus) [PDF].
For detailed information about these and other aerodigestive disorders, see, for example, Andrews (2006), Ashland and Hersh (2009), Coyle (2010), Dinwiddie (2004), Jadcherla (2012), Matsuo and Palmer (2008), and Morris et al. (2006).
Speech-Language Pathologist (SLP) Involvement in Aerodigestive Disorders
Aerodigestive disorders can cause secondary problems in feeding, swallowing, voice, and/or laryngeal airway function. SLPs play a role in the screening, assessment, diagnosis, and treatment of these secondary problems and often work collaboratively with other professionals in providing services to individuals with aerodigestive disorders.
Paradoxical Vocal Fold Movement (PVFM)
Paradoxical vocal fold movement, or PVFM, is the intermittent, episodic adduction of the vocal folds during inspiration. During episodes, the vocal folds adduct partially or fully and restrict the passage of air to the lungs. PVFM can occur in isolation, or it can co-occur with other conditions, including pulmonary disorders (e.g., asthma), laryngeal abnormalities, and cardiac pathology (Reitz et al., 2014). About 29%–40% of those with PVFM also have asthma (Gurevich-Uvena et al., 2010). SLPs are involved in the diagnosis and direct behavioral management of PVFM.
Chronic Cough
Chronic cough is most commonly defined as a cough lasting more than 8 weeks in adults and more than 4 weeks in children (Asilsoy et al., 2008; Morice, 2004). Chronic cough may be termed “somatic cough syndrome” in the absence of a known cause or “tic cough” when it is accompanied by core clinical features of tics (e.g., suppressibility, distractibility, suggestibility, variability, and presence of a warning sensation; Vertigan, 2017). SLP intervention is an effective treatment for chronic cough (Gibson & Vertigan, 2009; Petty & Dailey, 2009) and addresses the management of cough regardless of the initiating cause.
The incidence of a disorder or condition refers to the number of new cases identified in a specified time period. Prevalence refers to the number of individuals who are living with the disorder or condition in a given time period.
The following aerodigestive disorders provide a sample of conditions that can cause feeding, swallowing, voice, and/or laryngeal airway problems that may involve treatment by a speech-language pathologist (SLP). Some problems may be symptomatic or indicative of an aerodigestive disorder but do not involve treatment by an SLP. For example, dysphagia symptoms in individuals with esophageal dysmotility may resolve following medical and/or surgical intervention.
Airway Disorders
- Laryngeal cleft occurs in 1 out of 10,000–20,000 infants, with slightly higher rates noted in males with a ratio ranging from 1.2:1.0 to 1.8:1.0 (Leboulanger & Garabédian, 2011). Approximately 41% of patients with laryngeal cleft were found to silently aspirate (Velayutham et al., 2017).
- Laryngomalacia was estimated to affect approximately 1 in 2,600–3,100 newborns, and stridor was a reported symptom in the majority of children in the study (Kusak et al., 2017). Estimates reported dysphagia to be present in 41%–50% of patients with laryngomalacia (Simons et al., 2016; Velayutham et al., 2017).
Pulmonary Tract Disorders
- Chronic obstructive pulmonary disease (COPD) was self-reported by 15.5 million adults in the United States (40.3 cases per 100,000 individuals). Higher prevalence was reported in rural areas (Croft et al., 2018). An increase in compromised swallowing function was reported for adults with COPD over 60 years of age (Ghannouchi et al., 2016).
- Paradoxical vocal fold movement (PVFM) has been associated with chronic cough (Vertigan, Gibson, et al., 2007) and asthma (Ciccolella et al., 1997). True prevalence of PVFM is unknown due to inconsistent diagnostic criteria and a lack of awareness of the disorder. However, studies have reported PVFM as a subset of the investigated clinical population. For example, PVFM was estimated to occur in 2.5%–22% of emergency room patients presenting with shortness of breath or asthma (Ciccolella et al., 1997; Jain et al., 1999).
- Across the life span, reports estimated that PVFM is more common in females than in males, with a ratio ranging from 2:1 to 3:1 (Brugman, 2003; Morris et al., 2006).
- Increased rates of PVFM were reported in elite athletes (Rundell & Spiering, 2003), in individuals with elevated stress (Dietrich et al., 2008), and in individuals exposed to irritants (e.g., reflux, allergens; Perkner et al., 1998).
Upper Digestive Tract Disorders
- Gastroesophageal reflux disease (GERD) is associated with many aerodigestive disorders, including, but not limited to, laryngeal cleft, esophageal atresia, and eosinophilic esophagitis (EoE). Estimates of GERD in individuals with esophageal disorders ranged from 40.2% (Connor et al., 2015) to 65.3% (Mansoor & Cooper, 2016) of patients. Voice disorders and dysphagia may also be associated with GERD. Voice disorders are reported to be 1.8 times higher in patients with GERD (Katz et al., 2013; Poelmans & Tack, 2005).
- Esophageal atresia/tracheoesophageal fistula was estimated to affect 2.3 out of 100,000 live births in 2017. Prevalence rates of long-term dysphagia in individuals with esophageal atresia ranged from 18.2% to 84.2% (with pooled estimated prevalence of 50.3%; Connor et al., 2015; Coppens et al., 2016). Prevalence of dysphagia decreases as children get older (Coppens et al., 2016), but dysphagia has been commonly indicated in adults who had esophageal atresia repair as children (Taylor et al., 2007).
- Eosinophilic Esophagitis (EoE) was estimated to affect 71.1 out of 100,000 children and 25.9–55.5 out of 100,000 adults (Mansoor & Cooper, 2016; Maradey-Romero et al., 2015), with a prevalence rate significantly higher in adult men than in adult women (35.8 vs. 17.8 out of 100,000 persons, respectively). Relative to other races and ethnicities, EoE was highest in Caucasians. EoE was estimated to affect 18.6 out of 100,000 elderly persons (Maradey-Romero et al., 2015).
- Patients with EoE reported dysphagia as a common symptom. Dysphagia was reported in 46.2%–94.5% of adults (Shaheen et al., 2018). Estimates reported that 4.8%–60.9% of children with EoE experience dysphagia and globus sensation, but estimates may be as high as 88% (Soon et al., 2013).
Voice and swallowing problems commonly occur as a result of structural or physiologic changes to the aerodigestive tract secondary to surgery or radiation therapy. For example, the majority of individuals (70.5%) who received a lung transplant and subsequent swallowing evaluation showed laryngeal penetration or aspiration (Atkins et al., 2010). Following an esophagectomy, the incidence of vocal fold paralysis/paresis was estimated to be 1.96% of individuals, with 35% of those individuals receiving speech-language pathology services (Crowson et al., 2018). For more information, visit ASHA's Practice Portal pages on Head and Neck Cancer, Dysphagia (Adult), and Voice Disorders.
Signs are observations made by a third party (e.g., clinician or family member). For example, observations of coughing when someone swallows may be a sign of aspiration, and observations of changes in someone's vocal pitch may be a sign that the vocal folds are swollen or inflamed.
Symptoms are a person's own perception of changes in their swallowing, voice, breathing, or desire to eat or drink. Symptoms are usually described in terms of severity, location, frequency, and duration. For example, a person may notice that, recently, they have been coughing a great deal following exercise.
Signs and symptoms of aerodigestive disorders can vary depending on the specific disorder and the severity of the condition causing the disorder.
The following signs and symptoms are grouped by the function that can be affected:
Feeding and Swallowing
- aversion, disinterest, or refusal behaviors surrounding eating or drinking
- avoidance of certain foods and/or food characteristics
- avoidance of eating and drinking in public
- coughing or choking during or after eating
- globus sensation (feeling of something stuck in the pharynx)
- increased duration of feeding and/or mealtimes
- increased swallowing effort
- odynophagia (painful swallowing)
- pharyngonasal backflow (often referred to as “nasopharyngeal reflux”)
- poor weight gain in infants and children
- recurrent pulmonary infections, such as pneumonia
- regurgitation of swallowed food back into the pharynx or into the oral or nasal cavity
- slow or uncoordinated feeding in infants and children
- throat clearing during or after eating
- unexplained weight loss in adults or children
- wet breath sounds or wet vocal quality during or after eating
Voice
- aphonia (no voicing)
- breathiness
- increased vocal effort
- pain while voicing (odynophonia)
- rough vocal quality
- strained vocal quality
- vocal fatigue
- vocal pitch changes (e.g., in response to inflammation and edema)
- weak or inadequate vocal volume
Respiration
- chronic cough
- discoordinated or weak voluntary cough
- excessive mucous secretion
- excessive sputum production
- inability to manage oral and/or pharyngeal secretions independently
- increased effort of breathing
- overwhelming need to want to “take a breath”
- pneumonia
- rapid respiratory rate
- recurrent respiratory infections
- stridor (secondary to vocal fold paralysis or other airway obstruction; inspiratory or biphasic)
- weak reflexive cough
- wheezing
Paradoxical Vocal Fold Movement (PVFM)
- cough and rough vocal quality before or during an episode of vocal fold adduction
- difficulty inhaling, exhaling, or both (sole report of difficulty exhaling suggests asthma)
- lightheadedness that resolves quickly when trigger is removed
- stridor on inhalation (stridor for both inhalation and exhalation suggests laryngeal obstruction)
- sudden adduction of the vocal folds induced by triggering stimuli, such as activity, stress, or environmental irritants
- sudden and total loss of voice
- tightness in the throat
Chronic Cough
- productive (wet) or nonproductive (dry) cough
- cough lasting more than 8 weeks in adults and more than 4 weeks in children
For more detailed information about the signs and symptoms of aerodigestive disorders, see, for example, Andrews (2006), Ashland and Hersh (2009), Coyle (2010), Dinwiddie (2004), Ibrahim et al. (2007), Jadcherla (2012), Matsuo and Palmer (2008), Morice (2004), and Morris et al. (2006).
There are many ways to categorize the causes of aerodigestive disorders, given the overlap of structures and functions involved.
This Practice Portal page uses the following categories:
Congenital
- embryologic origins, including incomplete or atypical development, innervation, structure, and function of the aerodigestive tract structures
Structural/Anatomical
- injury or surgery affecting airway, pulmonary, or digestive structure and function
- weakness or dysfunction of the upper esophageal sphincter, allowing for regurgitation of acidic content into the pharynx, larynx, or nasal airway
- weakness or dysfunction of the lower esophageal sphincter, allowing acidic stomach contents to reenter the esophagus
Functional
- emotional stressors, fear, and/or anxiety that contribute to increased muscle tension
- environmental irritants or exercise
- laryngeal hyperreactivity
- laryngotracheal hyporeactivity
Other Medical Conditions
- autonomic dysfunction (e.g., diabetic neuropathy, vasovagal syncope)
- cardiovascular, pulmonary, or neurological diseases, or cancer, leading to breathing–swallowing incoordination (e.g., congenital heart defects, meconium aspiration syndrome, chronic lung disease, cystic fibrosis, head and neck cancer, motor neuron disease)
- irregular, unsynchronized, inappropriate, or absent esophageal contractions causing motility problems
- neurological diseases affecting aerodigestive sensorimotor function (e.g., stroke, Parkinson's disease, prematurity, hypoxic ischemic encephalopathy, cerebral palsy, muscular dystrophy, myopathies)
- neurological problems that trigger coughing, laryngospasm, bronchial constriction, or long-term bronchial changes affecting lung function
- recovery from respiratory failure or aerodigestive disuse during periods of critical care due to the use of artificial airways
Paradoxical Vocal Fold Movement (PVFM)
The exact cause of PVFM is not known, although PVFM may be related to laryngeal hyperresponsiveness.
PVFM may be triggered by
- organic factors, such as gastroesophageal reflux or environmental irritants, or
- nonorganic factors, such as exercise or psychological stress.
Chronic Cough
- asthma syndrome
- esophageal diseases, such as gastroesophageal reflux
- idiopathic heightened cough response, particularly in females
- rhinitis and sinusitis
- postnasal drip
- use of angiotensin-converting enzyme inhibitors (medications for the treatment of high blood pressure and heart failure)
For detailed information about the causes of aerodigestive disorders, see, for example, Andrews (2006), Ashland and Hersh (2009), Coyle (2010), Dinwiddie (2004), Ibrahim et al. (2007), Jadcherla (2012), Matsuo and Palmer (2008), Morice (2004), Morris et al. (2006), and Reitz et al. (2014).
Speech-language pathologists (SLPs) play a central role in the screening, assessment, diagnosis, and treatment of feeding, swallowing, voice, and laryngeal airway problems related to aerodigestive disorders. The professional roles and activities in speech-language pathology include clinical/educational services (diagnosis, assessment, planning, and treatment); prevention and advocacy; and education, administration, and research. See ASHA's Scope of Practice in Speech-Language Pathology (ASHA, 2016).
Appropriate roles for SLPs include, but are not limited to, the following:
- Screening of individuals who present with signs and symptoms (e.g., feeding, swallowing, voice, and laryngeal airway function) that are consistent with aerodigestive disorders and determining the need for further assessment and/or referral to other services.
- Conducting a comprehensive assessment of feeding, swallowing, voice, and respiration patterns associated with aerodigestive disorders, both clinically and instrumentally.
- Ensuring the cultural and linguistic appropriateness of diagnostic and treatment procedures (see ASHA's Practice Portal pages on Cultural Responsiveness, Multilingual Service Delivery in Audiology and Speech-Language Pathology, and Collaborating With Interpreters, Transliterators, and Translators).
- Diagnosing impairments in feeding, swallowing, voice, and laryngeal airway functions that are associated with aerodigestive disorders.
- As an essential member of a multidisciplinary team, contributing to the diagnosis of paradoxical vocal fold movement (PVFM) and helping to differentiate PVFM from other conditions and disorders.
- Serving as an integral member of a team of physicians and other professionals working with individuals with aerodigestive disorders and their families/caregivers (see ASHA's resource on collaboration and teaming).
- Making evidence-based recommendations about the management of feeding, swallowing, voice, and laryngeal airway problems related to aerodigestive disorders in collaboration with the patient, family, and interprofessional treatment team. (see ASHA's resources on interprofessional education/interprofessional practice [IPE/IPP] and person- and family-centered care).
- Recommending referrals outside of the aerodigestive team for further diagnosis or treatment based on patient needs.
- Developing person-centered treatment plans that account for patient/family values and expectations as well as adapting treatment plans to accommodate patient preferences (see ASHA's resource on person- and family-centered care).
- Educating and counseling persons with aerodigestive disorders and their families regarding feeding, swallowing, voice, and breathing-related issues, as well as facilitating participation in family, vocational, and community contexts.
- Consulting and collaborating with other professionals to facilitate program development and to provide evaluation and/or expert testimony, as appropriate.
- Providing prevention information to individuals and groups known to be at risk for feeding, swallowing, voice, and/or laryngeal airway problems related to aerodigestive disorders.
- Advocating for individuals with feeding, swallowing, voice, and laryngeal airway problems related to aerodigestive disorders at the local, state, and national levels.
- Educating other professionals on the needs of persons with aerodigestive disorders and the role of SLPs in diagnosing and managing feeding, swallowing, voice, and laryngeal airway problems associated with aerodigestive disorders.
- Remaining informed of research and new developments in the area of aerodigestive disorders and helping advance the knowledge base related to the nature and treatment of feeding, swallowing, voice, and laryngeal airway problems associated with these disorders.
As indicated in the ASHA Code of Ethics (ASHA, 2023), SLPs who serve this population should be specifically educated and appropriately trained to do so. This includes maintaining and documenting the highest level of competence in the areas of practice and ensuring referral of patients to the most qualified practitioner in each area of practice in which the SLP is not highly qualified.
See the Assessment section of ASHA's Evidence Maps on Voice Disorders, Dysphagia (Adult), and Pediatric Feeding and Swallowing for pertinent scientific evidence, expert opinion, and client/caregiver perspectives.
Assessment and treatment of aerodigestive disorders may require use of appropriate personal protective equipment.
Most aerodigestive disorders are identified by a physician on the basis of physical examination and one or more of the following:
- gastrointestinal evaluation (e.g., esophageal motility study; gastric emptying test; esophagogastroduodenoscopy; esophagram; esophageal manometry; 24-hour pH or impedance test; Raman spectroscopy)
- instrumental examinations (e.g., endoscopy; videofluoroscopy; airway fluoroscopy; flexible bronchoscopy; bronchoalveolar lavage; direct microlaryngoscopy; high-resolution pharyngeal manometry)
- pulmonary function tests
- X-ray and other imaging studies (e.g., chest X-ray; chest computed tomography scan; magnetic resonance imaging; electromyography; ultrasound)
Assessment of impairments caused by aerodigestive disorders often requires a multidisciplinary approach involving the speech-language pathologist (SLP) and other medical, surgical, and rehabilitation specialists. In collaboration with other health care specialists, the SLP provides expertise on feeding, swallowing, voice, and laryngeal airway problems related to aerodigestive disorders.
These collaborations may be a part of an established aerodigestive disorders team or may occur as a result of informed, targeted referrals within or outside the SLP's area of expertise. See ASHA's resources on interprofessional education/interprofessional practice [IPE/IPP] and collaboration and teaming.
A multidisciplinary approach may include
- a team of medical and other professionals,
- team meetings,
- combined assessment procedures,
- care coordination, and
- follow-up clinic visits.
A core multidisciplinary team may include one or more of the following professionals:
- allergist
- anesthesiologist
- gastroenterologist
- nurse
- nurse practitioner
- oncologist
- otolaryngologist
- physician assistant
- primary care physician (pediatrician in the case of a child, geriatrician in the case of elderly patients)
- pulmonologist
- registered dietitian
- SLP
Depending on the age of the individual and the specific concerns, other team members may include the following:
- cardiologist
- coach/athletic trainer
- medical geneticist
- neurologist
- occupational therapist
- physical therapist
- psychologist
- radiologist
- respiratory therapist
- sleep specialist
- social worker or case manager
- sports medicine physician
- surgeon
See Boesch et al. (2018) and Piccione and Boesch (2018).
Person- and Family-Centered Care
Person- and family-centered care is a collaborative approach grounded in a mutually beneficial partnership among individuals, families, and clinicians. Each party is equally important in the relationship, and each party must respect the knowledge, skills, and experiences that the others bring to the process. This approach incorporates individual and family preferences and priorities and offers a range of services, including
- providing counseling and emotional support,
- providing information and resources,
- coordinating services,
- teaching specific skills to facilitate communication, and
- advocating for services.
See ASHA's resource on person- and family-centered care.
Screening by an SLP
An SLP may be the first to see an individual who is experiencing voice or swallowing problems. These individuals may or may not have an underlying aerodigestive disorder. The purpose of screening is to identify individuals who require further assessment by an SLP or referral for other professional services. Screening may uncover findings that suggest underlying medical problems. See information about screening in the Assessment section of ASHA's Practice Portal pages on Voice Disorders, Dysphagia (Adult), and Pediatric Feeding and Swallowing.
It is important for SLPs to
- be familiar with anatomical structures affected by various aerodigestive disorders;
- be familiar with changes in feeding, swallowing, voice, and respiration problems that can be caused by aerodigestive disorders;
- recognize deviations in structure and function that warrant an aerodigestive evaluation by a physician; and
- make appropriate referrals, as needed.
SLPs screen for the following observed and reported changes:
- Voice and respiration
- vocal quality (e.g., rough voice, strained voice)
- vocal effort (e.g., vocal fatigue, report of pain while voicing)
- presence of stridor or labored breathing that affects breath support for voicing
- rapid respiratory rate
- chronic cough
- Swallowing and dietary changes
- clinical signs of feeding and swallowing problems (e.g., coughing, throat clearing, discomfort or globus sensation when swallowing
- other indicators such as poor weight gain in infants and unintentional weight loss in adults, or purposeful avoidance of previously enjoyed liquids or foods
SLPs also look for signs of neurologic conditions (e.g., abnormal sensorimotor function) that can affect voice, swallowing, or respiration, or that signal an underlying medical condition.
If screening results indicate feeding, swallowing, or respiratory difficulties that suggest an underlying disease process, referral is made to an appropriate medical professional.
Comprehensive Assessment
Aerodigestive disorders may involve the interaction of multiple systems, including laryngeal, pulmonary, phonatory, digestive, and sensorimotor. Individuals may present with multiple complaints and varied symptoms. A thorough case history and sign/symptom assessment—gathered by members of a multidisciplinary team that includes an SLP—facilitate assessment and differential diagnosis.
Consistent with the World Health Organization's International Classification of Functioning, Disability and Health framework (ASHA, 2016a; World Health Organization, 2001), comprehensive assessment is conducted to identify and describe
- impairments in body structure and function, including those related to aerodigestive disorders and the effect of impairments in feeding, swallowing, voice, and laryngeal airway function;
- limitations in activity and participation, including functional communication and social interactions;
- contextual (environmental and personal) factors that serve as barriers to or facilitators of successful communication and life participation; and
- the impact of feeding, swallowing, voice, and laryngeal airway problems on quality of life, including the impact of limitations on the individual's social roles within their community.
See ASHA's resources titled Person-Centered Focus on Function: Voice [PDF], Person-Centered Focus on Function: Adult Swallowing [PDF], and Person-Centered Focus on Function: Pediatric Feeding and Swallowing [PDF] for examples of handouts featuring assessment data consistent with the International Classification of Functioning, Disability and Health framework.
Comprehensive Assessment: Focus on Components Completed by the SLP
Case History (in Conjunction With Team)
- medical history (e.g., birth history, developmental history, history of digestive conditions, hospitalizations, recurrent pneumonia or respiratory infections, new onset of bronchitis, stroke or other neurological diseases)
- surgical history, including frequency and duration of intubation
- social history (e.g., education, employment)
- instrumental assessment history
- current medications
- exercise and activity habits, including identified triggers of respiratory problems
- dietary habits and nutritional status
- history of constipation
- changes in weight or failure to gain weight
- allergies that might affect voice, swallowing, and laryngeal airway function
- prior history of voice, swallowing, or airway problems, including prior assessment and treatment
Consider factors related to the anatomy and physiology of the aerodigestive tract and the age of the client.
Areas of Concern (in Conjunction With Team)
- presenting complaints (see the Signs and Symptoms section)
- patterns and progression of symptoms, both across time and within an episode (e.g., antecedent behaviors, recovery patterns, variability of symptoms)
- patient or caretaker perception of the severity of their symptoms
- patient goals
- report of variability in symptoms (e.g., intermittent voice change, intermittent reflux)
- report of environmental or activity-based triggers
- voice concerns/changes
- swallowing or feeding difficulties
Orofacial Sensorimotor Examination
- symmetry and movement of structures of the face, oral cavity, oropharynx, head, and neck during rest, during nonspeech tasks, and during speech/swallowing tasks
- sensory response to mechanical stimulation of the face, oral structures, and pharyngeal structures
- sensory response to taste, smell, and temperature
- review of reported laryngeal sensations (dryness, tickling, burning, pain, etc.)
Respiration
- respiratory pattern (abdominal, thoracic, clavicular), rate, rhythmicity
- coordination of respiration with phonation
- coordination of respiration with swallowing
- phrase length and other speech signs of impaired respiratory rate or tidal volume
- strength of volitional cough
Assess under varied conditions, including while at rest, during light activities such as walking, in challenging conditions such as aerobic activities, or during patient-identified trigger activities.
Voice
- auditory–perceptual assessment (subjective)
- voice quality—including roughness, breathiness, strain, pitch, and loudness
- phonation—including voice onset/offset and the ability to sustain voice during speech
- formal acoustic and aerodynamic measures
- instrumental assessment
- laryngoscopy—measures structure and gross function (using flexible or rigid videoendoscopy)
- stroboscopy—measures vibratory function (using flexible or rigid endoscopy)
See the Assessment section of ASHA's Practice Portal page on Voice Disorders for detailed information.
Feeding and Swallowing
- clinical evaluation of feeding and swallowing
- instrumental assessment
- Fiberoptic endoscopic evaluation of swallowing
- videofluoroscopic swallowing study (also known as “modified barium swallow study” or MBSS)
- high-resolution pharyngeal manometry
See the Assessment section of ASHA's Practice Portal pages on Dysphagia (Adult) and Pediatric Feeding and Swallowing for detailed information.
Cultural and Individual Considerations
SLPs conduct assessments in a manner that is sensitive to the individual's cultural background, religious beliefs, dietary beliefs/practices/habits, history of disordered eating behaviors, and preferences for medical intervention. Cultural, religious, and individual beliefs about food and eating practices may affect an individual's comfort level or willingness to participate in assessment. Some eating habits that appear to be a sign or symptom of an aerodigestive disorder (e.g., avoiding certain foods or refusing to eat in front of others) may, in fact, be related to cultural differences in meal habits or may be symptoms of an eating disorder (National Eating Disorders Association, n.d.).
Individual beliefs and preferences are considered when providing education and recommendations. Ethnographic interviewing strategies can help in gathering useful information (Westby et al., 2003). Collaboration with other professionals (e.g., cultural broker, mental health provider, registered dietitian, etc.) may be beneficial. See ASHA's Practice Portal pages on Cultural Responsiveness and Collaborating With Interpreters, Transliterators, and Translators for more information.
Additional Considerations
When completing videofluoroscopic swallow assessments, SLPs need to consider the potential impact of the barium concentration and viscosity of the test stimuli for all individuals. This is particularly important for infants and young children with aerodigestive disorders.
Using the appropriate weight per volume of barium concentrate reduces residual coating, which may affect the diagnosis or interpretation of the study. Viscosity of test fluids should approximate the customary or recommended fluid consistency as closely as possible (Cichero et al., 2011; Dodrill & Gosa, 2015). Use of a standardized flow test ensures that the tested consistency matches the defined consistency.
Potential interventions and treatment recommendations (positioning, utensils, bottle and nipple types, textures and liquid viscosity, and compensatory strategies) should be assessed during the examination. See the Assessment section of ASHA's Practice Portal pages on Dysphagia (Adult) and Pediatric Feeding and Swallowing for more details.
Paradoxical Vocal Fold Movement (PVFM)
Differential diagnosis of PVFM involves a multidisciplinary approach (Koufman & Block, 2008). Team members may include pulmonologists, allergists, otolaryngologists, gastroenterologists, cardiologists, psychologists, and SLPs (Altman et al., 2000). The SLP is an important member of the team and plays an essential role in diagnosis. They obtain a detailed case history, assess breathing patterns, perform a skilled fiberoptic laryngoscopy, and synthesize test information from all other team members (Reitz et al., 2014).
The SLP gathers the following case history information:
- onset of breathing difficulty—triggers (e.g., allergies and gastroesophageal reflux), duration, sensation, description, attempted treatments, and response
- frequency and length of PVFM attacks
- respiratory struggle during physical exertion
- gastroesophageal reflux
- respiratory allergies
- perception of excessive or different vocal effort
Assessment activities may include the following:
- Observation of breathing pattern at rest or during quiet activity.
- Fiberoptic laryngoscopy (Ibrahim et al., 2007), with nasendoscopy preferred to assess
- structural and functional integrity of the vocal folds;
- laryngeal dynamics across a range of activities;
- breathing patterns at rest and during dyspnea when/if trigger is known
- airway for paradoxical adduction of the true vocal folds with or without involvement of supraglottic structures, present during inhalation (partial adduction of the vocal folds during exhalation is typical for asthma); an
- the presence of a posterior glottal gap usually during inhalation (Morris et al., 2006) with a diamond-shaped glottic gap.
Note: It may be possible to have an asymptomatic larynx and still meet the criteria for PVFM (Olin et al., 2014).
Chronic Cough
The SLP helps in the differential diagnosis of chronic cough by gathering a detailed case history, performing fiberoptic laryngoscopy, and assessing voice.
For patients presenting with chronic cough, the SLP gathers information about
- the presence of associated causes of the cough, such as gastroesophageal reflux, postnasal drip, asthma, use of angiotensin-converting enzyme inhibitors or other medications, and smoking;
- characteristics of the cough—description, pattern, perceived warning of onset, perception of control of the cough, strategies to control the cough and effectiveness of those strategies;
- the degree of concern about the cough;
- the onset, duration, and progression of the cough;
- previous treatment for the cough and results of the treatment; and
- quality-of-life issues (social isolation, pain, or injury) secondary to the cough (Vertigan, Theodoros, et al., 2007).
Assessment activities may include
- laryngeal visualization;
- observation of breathing patterns and neck/muscle tension; and
- voice assessment, including perceptual description of the voice, discussion of concerns related to voice, and activities such as sustained phonation and pitch glides that may elicit cough.
See the Treatment section of ASHA's Evidence Maps on Voice Disorders, Dysphagia (Adult), and Pediatric Feeding and Swallowing for pertinent scientific evidence, expert opinion, and client/caregiver perspectives.
Decisions about goals and treatment options are made in partnership with the person, their family/caregiver, and other caregiving professionals. As part of a multidisciplinary team (see the Assessment section above), the speech-language pathologist (SLP) may be involved in assessing the individual's response to medical treatment and in implementing both indirect and direct strategies during or following medical treatment. See ASHA's resources on interprofessional education/interprofessional practice [IPE/IPP] and person- and family-centered care.
Comprehensive multidisciplinary treatment of aerodigestive disorders may include
- medical management (including pharmacotherapy and/or surgery) of underlying causes;
- indirect or compensatory treatment via environmental, dietary, and lifestyle modification; and
- direct or restorative intervention via voice, swallowing, and/or laryngeal airway treatment by an SLP.
Medical Management
Medical management decisions in aerodigestive disorders balance airway needs for breathing with optimal preservation of vocal quality and swallowing integrity (Dinwiddie, 2004). Approaches vary from “wait and watch” to complex surgical interventions.
Examples of medical approaches by appropriate medical professionals include, but are not limited to, the following:
- endoscopic treatment of structural abnormalities (e.g., dilation)
- medical or surgical management of the underlying disease/condition leading to the aerodigestive disorder
- surgical repair of structural abnormalities affecting aerodigestive function (e.g., arytenoidopexy, fundoplication, laryngeal cleft repair, supraglottoplasty, arytenoidectomy)
Dietary and Environmental Management
Dietary, compensatory, and environmental management may include the following:
- Dietary changes, such as
- implementing elimination diets,
- conducting food challenges (systematic introduction of new foods or textures),
- reducing acid-producing foods, and
- increasing water intake to hydrate the vocal folds and to support healthy phonation.
- Compensatory changes, such as
- using positional strategies while eating or drinking (e.g., elevating the head of the bed, turning the head) and
- implementing maneuver-based strategies when eating and drinking (e.g., supraglottic swallow).
- Environmental management, such as
- avoiding triggers (e.g., environmental pollutants, strenuous exercise).
Direct or Restorative Intervention
SLPs provide direct or restorative treatment to address functional voice problems (including respiratory support for voicing) and feeding and swallowing problems. SLPs also provide direct treatment for laryngeal airway problems, including paradoxical vocal fold movement (PVFM), and chronic cough.
The nature, scope, and duration of SLP management depend on
- the underlying aerodigestive disorder, structures and functions affected, severity, and relevant history;
- the type and course of medications to treat underlying and co-occurring diseases; and
- the type and extent of surgical management required (e.g., surgical intervention and healing time, need for a temporary feeding tube).
See ASHA's Practice Portal pages on Voice Disorders, Dysphagia (Adult), and Pediatric Feeding and Swallowing for specific treatment options and techniques related to these disorders.
See ASHA's resources titled Person-Centered Focus on Function: Voice [PDF], Person-Centered Focus on Function: Adult Swallowing [PDF], and Person-Centered Focus on Function: Pediatric Feeding and Swallowing [PDF] for examples of handouts featuring assessment data consistent with the International Classification of Functioning, Disability and Health framework.
Treatment Considerations for Pediatrics
Treatment selection depends on the child's age, cognitive and physical abilities, and specific swallowing and feeding problems. Treatment options—including postural and positioning techniques, maneuvers, and feeding strategies—are discussed in detail in the Pediatric Feeding and Swallowing Practice Portal page.
Infants and young children with aerodigestive disorders may benefit from alterations of liquid viscosity to improve airway protection during swallowing and/or to reduce the impact of reflux when tube feeding. This may include the use of natural foods or commercial dietary thickening agents to increase liquid viscosity. When making such recommendations, SLPs should consult with the medical team and be aware of the possible impact of thickening agents on nutritional status and overall health. For example, the addition of a thickener may alter the nutritional composition of the formula or breast milk. This may require the child to ingest more volume in order to obtain the necessary nutrients, or it may provide more than the recommended calories or the amount of certain nutrients (e.g., more than the recommended iron, if rice cereal is the thickening agent).
In addition, children with a history of necrotizing enterocolitis are advised to avoid gel-based thickeners containing the agent xanthan gum. Food allergies must also be considered when thickening agents are being considered.
Precaution
The U.S. Food and Drug Administration (FDA) has cautioned consumers about using commercial, gum-based thickeners for infants from birth to 1 year of age, especially when using the product to thicken breast milk. SLPs should be aware of these cautions and consult, as appropriate, with their facility to develop guidelines for using thickened liquids with infants. See FDA consumer cautions (FDA, 2017).
See also the Treatment section of ASHA's Evidence Map on Pediatric Feeding and Swallowing. Use keywords “Diet Modifications” and “Early Intervention.”
Intervention for PVFM
The goal of treatment is to establish consistent vocal fold abduction during the breathing cycle to maintain a patent airway. This reduces anxiety and affirms that breathing is consistently achievable, even in the presence of environmental or activity-related triggers.
Behavioral management by an SLP is the preferred treatment approach to PVFM (Reitz et al., 2014). Other disciplines may also be involved in treatment (e.g., medical intervention to treat reflux or allergy triggers, when present).
SLPs may implement the following procedures with most individuals with PVFM. Procedures are individualized based on triggers or other factors (Mathers-Schmidt, 2001; Sandage & Zelazny, 2004) and include the following:
- Relaxed throat breathing—trains the vocal folds to abduct and remain abducted throughout the breathing cycle. Techniques include
- sniffing in through the nose with the tongue relaxed on the floor of the mouth and the lips gently touching, followed by exhalation through pursed lips or the production of a strident sound such as /s/, an
- sipping air in through pursed lips, followed by an exhalation through pursed lips or the production of a strident sound such as /s/.
- Diaphragmatic/abdominal breathing—trains attention to expansion of the lower rib cage and abdomen during inhalation to avoid clavicular breathing patterns and shoulder/neck tension.
Once the individual has identified their most effective breathing technique, the SLP may introduce challenges (triggers) while using the technique. These include the following:
- Sports or exercise-specific training—implementing breathing techniques during a routine exercise activity or competitive sports training
- Training in the presence of environmental triggers (if applicable)—implementing breathing techniques during exposure to odors or other environmental triggers, beginning with non-noxious stimuli and progressing through noxious stimuli
See Reitz et al. (2014), Blager (2006), and Murry et al. (2006) for intervention details.
Intervention for Chronic Cough
The goal of treatment is to help the individual manage their cough by identifying triggers, using strategies to suppress the cough, reducing laryngeal irritation, and using healthy vocal hygiene behaviors (Vertigan, Theodoros et al., 2007). Speech-language services should be coordinated with medical management of the underlying cause; services should be implemented after ruling out or addressing other contributing factors (Murry et al., 2006).
Treatment activities include the following:
- Educating the individual about chronic cough and its treatment, including
- discussing the difference between acute cough and chronic cough, emphasizing that chronic cough does not have physiological benefits;
- establishing cough suppression as a safe and achievable goal;
- defining the cough trigger threshold and desensitization of the cough response; and
- emphasizing the importance of adhering to medications prescribed by physicians to manage cough.
- Implementing healthy vocal hygiene practices to maximize hydration and reduce irritation of the vocal folds, including helping the individual
- identify behaviors that are contributing to the cough (e.g., poor hydration, mouth breathing) and
- practice healthy vocal hygiene behaviors (e.g., drinking plenty of water and talking at moderate volume).
- Teaching cough suppression strategies (as appropriate), including
- monitoring the cough precursor or trigger;
- using relaxed throat breathing or prolonged, slow exhalation (see PVFM above);
- using pursed-lip breathing; and
- substituting coughing with other behaviors or distractions such as
- sucking on ice or non-medicated candy and
- swallowing dry or with sips of water.
The SLP typically introduces strategies without the presence of triggers to establish functional behaviors and to determine the person's most consistent response. The SLP may then introduce stimulants such as strong odors, increased activity levels, or other identified triggers to help the individual use the strategies before the “need” to cough. Treatment ends when the person can manage cough across a variety of contexts and in the presence of triggers.
See Blager et al. (1988), Petty and Dailey (2009), Soni et al. (2017), Vertigan (2017), and Vertigan, Theodoros et al. (2007).
Billing for PVFM and Chronic Cough Services
Providing appropriate procedure codes for evaluation and treatment is an important aspect of successfully billing for services. Payer policies often outline specific coverage guidelines and list relevant Current Procedural Terminology (CPT; American Medical Association, 2018) codes from the International Classification of Diseases and Related Health Problems (10th Revision, Clinical Modification; World Health Organization, 2015).
Although individuals with PFVM or chronic cough may not present with dysphonia, respiratory and laryngeal function are substrates of the speech system. SLPs use diagnostic and procedure codes for assessment and treatment of voice to represent these services. Payer policies regarding the coverage of PVFM and chronic cough vary. SLPs working with private insurance should verify coverage on the basis of each individual.
For more information about coding, see the following ASHA resources:
New CPT Evaluation Codes for SLPs
Medicare CPT Coding Rules for Speech-Language Pathology Services
Coding for Reimbursement Frequently Asked Questions: Speech-Language Pathology
Service Delivery
In addition to determining the type of treatment that is optimal for individuals with feeding, swallowing, voice, and laryngeal airway problems related to aerodigestive disorders, SLPs consider other service delivery variables—including format, provider, dosage, timing, and setting—that may affect treatment outcomes.
- Format—whether a person is seen for treatment one-on-one (i.e., individual) or as part of a group. The format of service delivery for this population can include in-person and telepractice models.
- Provider—the person administering the treatment (e.g., SLP, trained volunteer, caregiver).
- Dosage—the frequency, intensity, and duration of service.
- Timing—when intervention occurs relative to the diagnosis. This includes the timing of behavioral intervention in relation to surgical/physical management.
- Setting—the location of treatment (e.g., inpatient, outpatient, home, community based, sports venue).
ASHA Resources
- Aerodigestive Disorders of the Airway (Pharynx and Larynx) [PDF]
- Aerodigestive Disorders of the Pulmonary Tract (Trachea, Bronchi, and Lungs) [PDF]
- Aerodigestive Disorders of the Upper Digestive Tract (Esophagus) [PDF]
- Aerosol Generating Procedures
- Coding for Reimbursement Frequently Asked Questions: Speech-Language Pathology
- Collaboration and Teaming
- Cough: A Review of Anatomy and Physiology
- Frequently Asked Questions: Swallowing and Feeding (Dysphagia)
- Information for the Public: Chronic Cough
- Information for the Public: Paradoxical Vocal Fold Movement (PVFM)
- International Dysphagia Diet Standardisation Initiative (IDDSI)
- Interprofessional Education/Interprofessional Practice (IPE/IPP)
- Medicare CPT Coding Rules for Speech-Language Pathology Services
- New CPT Evaluation Codes for SLPs
- Palliative and End-of-Life Care
- Person- and Family-Centered Care
- Person-Centered Focus on Function: Adult Swallowing [PDF]
- Person-Centered Focus on Function: Pediatric Feeding and Swallowing [PDF]
- Person-Centered Focus on Function: Voice [PDF]
- SLP's Role in Evaluation and Treatment of Cough Function
- Sniffs, Gasps, and Coughs – Irritable Larynx Syndrome Across the Lifespan
- The Impact of Prescribed Medication on Swallowing: An Overview
- Treatment for Cough: Two Sides to the Story
Other Resources
The list of resources is not exhaustive, and the inclusion of any specific resource does not imply endorsement from ASHA.
- Aerodigestive Society
- American Academy of Allergy, Asthma & Immunology
- American Society of Pediatric Otolaryngology
- Cough – American Thoracic Society [PDF]
- Cough – CHEST Foundation
- Dysphagia Research Society
- Evidence-Based Systematic Review: Oropharyngeal Dysphagia Behavioral Treatments. Part V—Applications for Clinicians and Researchers [PDF]
- National Foundation of Swallowing Disorders
- National Institute on Deafness and Other Communication Disorders
- Pediatric Feeding Association
- RCSLT: New Long COVID Guidance and Patient Handbook
- Society for Ear, Nose, and Throat Advances in Children (SENTAC)
- The National Center for Voice & Speech
- The North American Airway Collaborative
Altman, K. W., Mirza, N., Ruiz, C., & Sataloff, R. T. (2000). Paradoxical vocal fold motion: Presentation and treatment options. Journal of Voice, 14(1), 99–103.
American Medical Association. (2018). CPT/Current Procedural Terminology (Professional Edition).
American Speech-Language-Hearing Association. (2016). Scope of practice in speech-language pathology [Scope of practice]. www.asha.org/policy/
American Speech-Language-Hearing Association. (2023). Code of ethics [Ethics]. www.asha.org/policy/
Andrews, M. L. (2006). Manual of voice treatment: Pediatrics through geriatrics (3rd ed.). Thomson Delmar Learning.
Ashland, J. E., & Hersh, C. J. (2009). Pediatric swallowing disorders: The speech-language pathologist's perspective. In K. Haver, M. Brigger, S. Hardy, & C. J. Hartnick (Eds.), Pediatric aerodigestive disorders (pp. 377–400). Plural.
Asilsoy, S., Bayram, E., Agin, H., Apa, H., Can, D., Gulle, S., & Altinoz, S. (2008). Evaluation of chronic cough in children. Chest,134(6), 1122–1128.
Atkins, B. Z., Petersen, R. P., Daneshmand, M. A., Turek, J. W., Lin, S. S., & Davis, R. D., Jr. (2010). Impact of oropharyngeal dysphagia on long-term outcomes of lung transplantation. The Annals of Thoracic Surgery, 90(5), 1622–1628.
Blager, F. B. (2006). Vocal cord dysfunction. Perspectives on Voice and Voice Disorders, 16(1), 7–10.
Blager, F. B., Gay, M. L., & Wood, R. P. (1988). Voice therapy techniques adapted to treatment of habit cough: A pilot study. Journal of Communication Disorders, 21(5), 393–400.
Boesch, R. P., Balakrishnan, K., Acra, S., Benscoter, D. T., Cofer, S. A., Collaco, J. M., Dahl, J. P., Daines, C. L., DeAlarcon, A., DeBoer, E. M., Deterding, R. R., Friedlander, J. A., Gold, B. D., Grothe, R. M., Hart, C. K., Kazachkov, M., Lefton-Greif, M. A., Miller, C. K., Moore, P. E., . . . Wood, R. E. (2018). Structure and functions of pediatric aerodigestive programs: A consensus statement. Pediatrics, 141(3), e20171701.
Brugman, S. M. (2003). The many faces of vocal cord dysfunction: What 36 years of literature tell us. American Journal of Respiratory and Critical Care Medicine, 167(7), A588.
Ciccolella, D. E., Brennan, K. J., Borbely, B., & Criner, G. J. (1997). Identification of vocal cord dysfunction (VCD) and other diagnoses in patients admitted to an inner city university hospital asthma center. American Journal of Respiratory and Critical Care Medicine, 155(4), A82.
Cichero, J., Nicholson, T., & Dodrill, P. (2011). Liquid barium is not representative of infant formula: Characterisation of rheological and material properties. Dysphagia, 26(3), 264–271.
Connor, M. J., Springford, L. R., Kapetanakis, V. V., & Giuliani, S. (2015). Esophageal atresia and transitional care—step 1: A systematic review and meta-analysis of the literature to define the prevalence of chronic long-term problems. The American Journal of Surgery, 209(4), 747–759.
Coppens, C. H., van den Engel-Hoek, L., Scharbatke, H., de Groot, S. A. F., & Draaisma, J. M. T. (2016). Dysphagia in children with repaired oesophageal atresia. European Journal of Pediatrics, 175(9), 1209–1217.
Coyle, J. L. (2010). Ventilation, respiration, pulmonary diseases, and swallowing. Perspectives on Swallowing and Swallowing Disorders (Dysphagia), 19(4), 91–97.
Croft, J. B., Wheaton, A. G., Liu, Y., Xu, F., Lu, H., Matthews, K. A., Cunningham, T. J., Wang, Y., & Holt, J. B. (2018). Urban-rural county and state differences in chronic obstructive pulmonary disease—United States, 2015. Morbidity and Mortality Weekly Report, 67(7), 205–211.
Crowson, M. G., Tong, B. C., Lee, H.-J., Song, Y., Harpole, D. H., Jones, H. N., & Cohen, S. (2018). Prevalence and resource utilization for vocal fold paralysis/paresis after esophagectomy. The Laryngoscope, 128(12), 2815–2822.
Dietrich, M., Verdolini Abbott, K., Gartner-Schmidt, J., & Rosen, C. A. (2008). The frequency of perceived stress, anxiety, and depression in patients with common pathologies affecting voice. Journal of Voice, 22(4), 472–488.
Dinwiddie, R. (2004). Congenital upper airway obstruction. Pediatric Respiratory Reviews, 5(1), 17–24.
Dodrill, P., & Gosa, M. M. (2015). Pediatric dysphagia: Physiology, assessment, and management. Annals of Nutrition & Metabolism, 66(Suppl. 5), 24–31.
Ghannouchi, I., Speyer, R., Doma, K., Cordier, R., & Verin, E. (2016). Swallowing function and chronic respiratory diseases: Systematic review. Respiratory Medicine, 117, 54–64.
Gibson, P. G., & Vertigan, A. E. (2009). Speech pathology for chronic cough: A new approach. Pulmonary Pharmacology & Therapeutics, 22(2), 159–162.
Gurevich-Uvena, J., Parker, J. M., Fitzpatrick, T. M., Makashay, M. J., Perello, M. M., Blair, E. A., & Solomon, N. P. (2010). Medical comorbidities for paradoxical vocal fold motion (vocal cord dysfunction) in the military population. Journal of Voice, 24(6), 728–731.
Ibrahim, W. H., Gheriani, H. A., Almohamed, A. A., & Raza, T. (2007). Paradoxical vocal cord motion disorder: Past, present and future. Postgraduate Medical Journal, 83(977), 164–172.
Jadcherla, S. (2012). Pathophysiology of aerodigestive pulmonary disorders in the neonate. Clinics in Perinatology,39(3), 639–654.
Jain, S., Bandi, V., Zimmerman, J., Hanania, N., & Guntupalli, K. (1999). Incidence of vocal cord dysfunction in patients presenting to emergency room with acute asthma exacerbation. Chest, 116(4), 243S.
Katz, P. O., Gerson, L. B., & Vela, M. F. (2013). Guidelines for the diagnosis and management of gastroesophageal reflux disease. The American Journal of Gastroenterology, 108(3), 308–328.
Koufman, J. A., & Block, C. (2008). Differential diagnosis of paradoxical vocal fold movement. American Journal of Speech-Language Pathology, 17(4), 327–334.
Kusak, B., Cichocka-Jarosz, E., Jedynak-Wasowicz, U., & Lis, G. (2017). Types of laryngomalacia in children: Interrelationship between clinical course and comorbid conditions. European Archives of Oto-Rhino-Laryngology, 274(3), 1577–1583.
Leboulanger, N., & Garabédian, E.-N. (2011). Laryngo-tracheo-oesophageal clefts. Orphanet Journal of Rare Diseases, 6(1), 81.
Logemann, J. A. (1998). Evaluation and treatment of swallowing disorders (2nd ed.). Pro-Ed.
Mansoor, E., & Cooper, G. S. (2016). The 2010–2015 prevalence of eosinophilic esophagitis in the USA: A population-based study. Digestive Diseases & Sciences, 61(10), 2928–2934.
Maradey-Romero, C., Prakash, R., Lewis, S., Perzynski, A., & Fass, R. (2015). The 2011–2014 prevalence of eosinophilic oesophagitis in the elderly amongst 10 million patients in the United States. Alimentary Pharmacology and Therapeutics, 41(10), 1016–1022.
Mathers-Schmidt, B. A. (2001). Paradoxical vocal fold motion: A tutorial on a complex disorder and the speech-language pathologist's role. American Journal of Speech-Language Pathology, 10(2), 111–125.
Matsuo, K., & Palmer, J. B. (2008). Anatomy and physiology of feeding and swallowing: Normal and abnormal. Physical Medicine and Rehabilitation Clinics of North America, 19(4), 691–707.
Morice, A. H. (2004). The diagnosis and management of chronic cough. European Respiratory Journal, 24(3), 481–492.
Morris, M. J., Allan, P. F., & Perkins, P. J. (2006). Vocal cord dysfunction: Etiologies and treatment. Clinical Pulmonary Medicine, 13(2), 73–86.
Murry, T., Tabaee, A., Owczarzak, V., & Aviv, J. E. (2006). Respiratory retraining therapy and management of laryngopharyngeal reflux in the treatment of patients with cough and paradoxical vocal fold movement disorder. Annals of Otology, Rhinology & Laryngology, 115(10), 754–758.
National Eating Disorders Association. (n.d). Warning signs and symptoms: Common symptoms of an eating disorder. https://www.nationaleatingdisorders.org/warning-signs-and-symptoms
Olin, J. T., Clary, M. S., Connors, D., Abbott, J., Brugman, S., Deng, Y., Chen, X., & Courey, M. (2014). Glottic configuration in patients with exercise‐induced stridor: A new paradigm. The Laryngoscope, 124(11), 2568–2573.
Perkner, J. J., Fennelly, K. P., Balkissoon, R., Bartelson, B. B., Ruttenber, A. J., Wood, R. P., II, & Newman, L. S. (1998). Irritant-associated vocal cord dysfunction. Journal of Occupational and Environmental Medicine, 40(2), 136–143.
Petty, B. E., & Dailey, S. H. (2009). The collaborative medical and behavioral management of chronic cough. Perspectives on Voice and Voice Disorders, 19(2), 49–57.
Piccione, J., & Boesch, R. P. (2018). The multidisciplinary approach to pediatric aerodigestive disorders. Current Problems in Pediatric and Adolescent Health Care, 48(3), 66–70.
Poelmans, J., & Tack, J. (2005). Extraoesophageal manifestations of gastro-oesophageal reflux. Gut, 54(10), 1492–1499.
Reitz, J. R., Gorman, S., & Kegyes, J. (2014). Behavioral management of paradoxical vocal fold motion. Perspectives on Voice and Voice Disorders, 24(2), 64–70.
Robbins, J. (2011). Upper aerodigestive tract neurofunctional mechanisms: Lifelong evolution and exercise. Head & Neck, 33(S1), S30–S36.
Rundell, K. W., & Spiering B. A. (2003). Inspiratory stridor in elite athletes. Chest,123(2), 468–474.
Sandage, M. J., & Zelazny, S. K. (2004). Paradoxical vocal fold motion in children and adolescents. Language, Speech, and Hearing Services in Schools, 35(4), 353–362.
Shaheen, N. J., Mukkada, V., Eichinger, C. S., Schofield, H., Todorova, L., & Falk, G. W. (2018). Natural history of eosinophilic esophagitis: A systematic review of epidemiology and disease course. Diseases of the Esophagus, 31(8), doy015.
Simons, J. P., Greenberg, L. L., Mehta, D. K., Fabio, A., Maguire, R. C., & Mandell, D. L. (2016). Laryngomalacia and swallowing function in children. The Laryngoscope, 126(2),478–484.
Soni, R. S., Ebersole, B., & Jamal, N. (2017). Treatment of chronic cough: Single-institution experience utilizing behavioral therapy. Otolaryngology—Head & Neck Surgery, 156(1), 103–108.
Soon, I. S., Butzner, J. D., Kaplan, G. G., & deBruyn, J. C. C. (2013). Incidence and prevalence of eosinophilic esophagitis in children. Journal of Pediatric Gastroenterology and Nutrition, 57(1), 72–80.
Taylor, A. C. F., Breen, K. J., Auldist, A., Catto-Smith, A., Clarnette, T., Crameri, J., Taylor, R., Nagarajah, S., Brady, J., & Stokes, K. (2007). Gastroesophageal reflux and related pathology in adults who were born with esophageal atresia: A long-term follow-up study. Clinical Gastroenterology and Hepatology, 5(6),702–706.
U.S. Food and Drug Administration. (2017). FDA expands caution about SimplyThick.
Velayutham, P., Irace, A. L., Kawai, K., Dodrill, P., Perez, J., Londahl, M., Mundy, L., Dombrowski, N. D., & Rahbar, R. (2017). Silent aspiration: Who is at risk? The Laryngoscope, 128(8),1952–1957.
Vertigan, A. E. (2017). Somatic cough syndrome or psychogenic cough—what is the difference? Journal of Thoracic Disease, 9(3), 831–838.
Vertigan, A. E., Gibson, P. G., Theodoros, D. G., & Winkworth, A. L. (2007). A review of voice and upper airway function in chronic cough and paradoxical vocal cord movement. Current Opinion in Allergy and Clinical Immunology, 7(1), 37–42.
Vertigan, A. E., Theodoros, D. G., Winkworth, A. L., & Gibson, P. G. (2007). Chronic cough: A tutorial for speech-language pathologists. Journal of Medical Speech-Language Pathology, 15(3),189–206.
Westby, C., Burda, A., & Mehta, Z. (2003, April). Asking the right questions in the right ways: Strategies for ethnographic interviewing. The ASHA Leader, 8(8), 4–17.
World Health Organization. (2001). International Classification of Functioning, Disability and Health.
World Health Organization. (2015). International Classification of Diseases (10th rev., clinical modification).
Acknowledgements
Content for ASHA's Practice Portal is developed through a comprehensive process that includes multiple rounds of subject matter expert input and review. ASHA extends its gratitude to the following subject matter experts who were involved in the development of the Aerodigestive Disorders page:
- Joan C. Arvedson, PhD, CCC-SLP
- Maia N. Braden, MS, CCC-SLP
- James L. Coyle, PhD, CCC-SLP
- James Curtis, MS, CCC-SLP
- Kendrea Layne Garand, PhD, CScD, CCC-SLP
- Claire Kane Miller, PhD, CCC-SLP
- Katy S. Peck, MA, CCC-SLP
- Teresa Pitts, PhD, CCC-SLP
- Mary J. Sandage, PhD, CCC-SLP
- Shannon M. Theis, PhD, CCC-SLP
- Sherri K. Zelazny, MA, CCC-SLP
Citing Practice Portal Pages
The recommended citation for this Practice Portal page is:
American Speech-Language-Hearing Association. (n.d.). Aerodigestive Disorders. (Practice Portal). Retrieved month, day, year, from www.asha.org/Practice-Portal/Clinical-Topics/Aerodigestive-Disorders/.
Content Disclaimer: The Practice Portal, ASHA policy documents, and guidelines contain information for use in all settings; however, members must consider all applicable local, state and federal requirements when applying the information in their specific work setting.












