Case Study: IPP Team Helps Child With a Cleft Palate to Improve Feeding, Swallowing, and Speech Sound Production
Work Setting: Health Care Work Setting: Private Practice
Summary
A Cleft Palate Team collaborated across specialties to help a 13-month-old child with a history of cleft palate to improve feeding, swallowing, and speech sound production. The interprofessional team completed individual assessments, discussed results, and made recommendations for Sam and the family.
Meet the Team
Background
Sam is a 13-month-old child with a history of cleft palate that was repaired 6 weeks prior to the family’s visit to the Cleft Palate Program. Palate repair was delayed due to a history of feeding and swallowing difficulties that resulted in poor weight gain and eventual need for a gastrostomy tube. The parents brought Sam to this current team assessment and were eager to hear how Sam was healing since surgery; they hoped to begin working with Sam on eating and drinking more frequently by mouth.
How They Collaborated
Sam was seen by multiple members of the Cleft Palate Program, including the plastic surgeon, members of the feeding team (developmental pediatrician, speech-language pathologist [SLP], and registered dietician), an SLP focused on communication, an audiologist, and the team social worker. These team members completed individual assessments, discussed results, and made recommendations for Sam and the family.
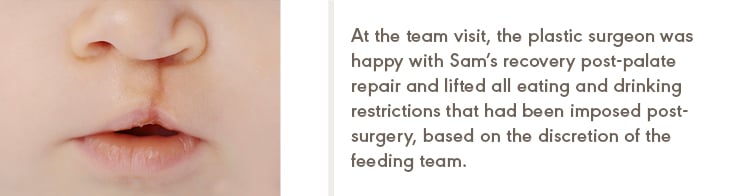
At the team visit, the plastic surgeon was happy with Sam’s recovery post-palate repair and lifted all eating and drinking restrictions that had been imposed post-surgery, based on the discretion of the feeding team. The feeding team was happy with Sam’s weight gain and gross motor developmental progress, and the SLP spent most of the visit (a) educating Sam’s parents about the results of a recent videofluoroscopic swallow study (VFSS) that showed aspiration with thin liquids and (b) assessing current function to help design a plan for home and local therapy to continue to advance feeding skills by mouth. The SLP demonstrated how to mix liquids to a mildly thick consistency, how to introduce and practice open- cup drinking, and how to model and encourage a more age-appropriate chewing pattern. Sam’s parents were given an opportunity to practice these skills and strategies, as well as written instructions for home use. Recommendations were to continue with local feeding therapy, incorporating strategies as given and advancing in therapy as appropriate.
The audiologist was happy with Sam’s testing after ear tubes were placed during the palate- repair surgery. Sam had a history of a bilateral conductive hearing loss, but after placement of tubes, his sound-field testing was within normal limits. Similarly, the team social worker had provided support to Sam’s parents throughout much of the medical care up to this visit; however, Sam’s parents denied having any current concerns or needs.
Unfortunately, Sam was seen by the SLP to evaluate his communication skills at the end of the clinic visit—and, by that time, Sam had fallen asleep. Parent report suggested age-appropriate receptive language skills, but concerns for expressive delays and a restricted speech sound inventory. Given the large amount of information that Sam’s parents were asked to digest and remember from today’s visit, the SLP focused on a few specific home strategies to encourage the development of oral consonants and to decrease the risk of developing compensatory articulation errors.
Outcome
Sam returned to the Cleft Palate Program a year later, close to Sam’s second birthday. The plastic surgeon continued to be happy with the progress and Sam was no longer followed by the feeding team as Sam had advanced to meeting the nutrition and hydration needs by mouth during that time. Speech and language skills continued to be delayed and were concerning for the development of glottal stop substitution errors. Given the minimal speech sound development that occurred over the past year, increased importance on collaboration with the local SLP and need for closer follow-up with the team SLP was discussed. Over the next few years, focus will be on speech and language development as well as Sam’s velopharyngeal function for speech, monitoring for resonance disorders and/or nasal air escape.
Ongoing Collaboration
Sam will continue to be assessed through the Cleft Palate Program through facial maturity, generally on an annual basis. Other medical professionals may be added to Sam’s team based on future needs or concerns.