Better Health Starts with Effective Communication
You prepare to examine a new patient. He tries to answer your questions about his medication tolerance and compliance, but you cannot understand what he is saying. You nod uncomfortably at your patient and then turn to continue the conversation with his daughter instead. Your patient becomes frustrated, especially because his daughter does not know about all of his current medications.
This scenario is familiar to many people who have communication disabilities—and maybe to you, as a provider. Lack of effective communication access for people with hearing, speech, language, voice, and/or cognitive difficulties can lead to frustration, wasted time, and less-than-optimal outcomes. What could the provider do differently?
Asking a patient about their communication needs FIRST can improve health care interactions and outcomes for patients, care partners, providers, and payers.
What is communication access?
Communication access means supporting individuals with communication disabilities so that they can effectively participate in and benefit from services and programs in the same way as people without communication disabilities. Effective communication occurs when each person in an interaction has equal opportunity to share, receive, and understand information in ways that work best for them, i.e., they have access to resources that best meet and support their communication needs.
Why does communication access matter?
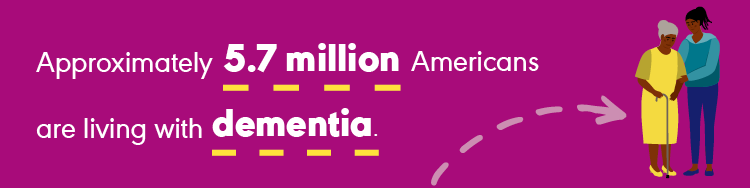
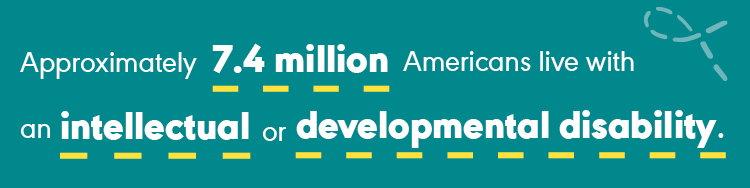
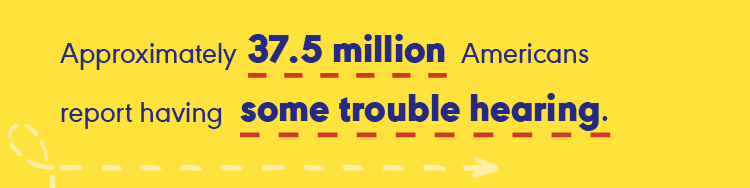
Simply put, effective communication is a human right! Effective communication benefits everyone's health and well-being. Communication access is especially critical for people with hearing, communication, and/or cognitive difficulties, who often experience barriers to care. When individuals with communication disabilities do not have access to the accommodations that they need, it can lead to adverse outcomes (Hurtig et al., 2018; Morris, 2022; Stransky et al, 2018; Stransky & Morris, 2019; Williams, 2021), including,
- poorer health,
- more chronic conditions,
- avoidance or delays in seeking care, and,
- increased health care costs (e.g., preventable adverse events due to lack of effective communication cost U.S. health care $29 billion annually).
Providing communication access using auxiliary aids and services ensures that interactions with people with communication disabilities are as effective as those with their peers without communication disabilities.
Be flexible with your communication style and your time based on each person’s needs. This can optimize patient safety, quality of care, costs, and treatment outcomes for people with hearing, communication, and/or cognitive difficulties.

Ask about communication preferences, strategies, and accommodations before start of care.

Communicate directly with the person (unless they indicate otherwise).

Check for understanding of information given and received.

Ensure environmental distractions are limited, and give your full attention.

Slow down to allow time to process information and respond.

Support interactions using different communication methods (gestures, writing, drawing, pictures, communication boards, videos, assistive technology).
Why should you support ACCESS?
When health care providers are sensitive to their patients’ communication needs and implement required accommodations and strategies for effective communication, it can improve patients'
- diagnostic accuracy
- understanding of treatment options
- informed consent
- supported decision-making
- adherence to care recommendations
- autonomy and participation in care
For the health care system, it can
lower hospital (re)admission rates
increase cost savings
improve safety metrics as well as adherence to standards and compliance
raise patient-provider satisfaction
What's your role?
Health care providers, policy makers, researchers, patients, and care partners need to collaborate in identifying and addressing barriers to effective communication to advance health equity and outcomes for people with communication disabilities. Learn more about Interprofessional Education (IPE) and Interprofessional Practice (IPP).
Be an ally!
Think about every interaction likely to occur with your patients and find ways to reduce any barriers to effective communication when
- Making appointments by phone or online
- Checking into appointments and filling out forms
- Interacting directly with patients, healthcare providers, and staff
- Reviewing exam results, treatment recommendations, prescriptions, patient education, and referrals
- Sharing billing and other documentation
Need help?
To learn more about communication disabilities and effective communication access, contact ASHA-certified audiologists and speech-language pathologists. To find a communication professional near you, visit ASHA's ProFind. Or call ASHA from 8:30 a.m.–5:00 p.m., Monday-Friday, at 800-638-8255.
We'd like your input to develop the communication access resources you need.
References
Hurtig, R. R., Alper, R. M., & Berkowitz, B. (2018). The cost of not addressing the communication barriers faced by hospitalized patients. Perspectives of the ASHA special interest groups, 3(12), 99–112.
Morris, M. A. (2022). Striving toward equity in health care for people with communication disabilities. Journal of Speech, Language, and Hearing Research, 65(10), 3623–3632.
Stransky, M., & Morris, M. (2019). Adults with communication disabilities face health care obstacles. The Asha Leader, 24(3), 46–55.
Stransky, M. L., Jensen, K. M., & Morris, M. A. (2018). Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. Journal of general internal medicine, 33, 2147-2155.
Williams, A. L. (2021). Interprofessional Advocacy for Health Care Equity. Leader Live.
 You prepare to examine a new patient. He tries to answer your questions about his medication tolerance and compliance, but you cannot understand what he is saying. You nod uncomfortably at your patient and then turn to continue the conversation with his daughter instead. Your patient becomes frustrated, especially because his daughter does not know about all of his current medications.
You prepare to examine a new patient. He tries to answer your questions about his medication tolerance and compliance, but you cannot understand what he is saying. You nod uncomfortably at your patient and then turn to continue the conversation with his daughter instead. Your patient becomes frustrated, especially because his daughter does not know about all of his current medications.