Ergonomic Case Study of an Audiologist Performing Visual Reinforcement Audiometry
September 2014
Chantal Trudel, BA, BID
Work-related injury and illness can cost individuals and employers time and money. Repetitive movements, poor posture, bending and lifting, and using pressure or force can contribute to various disorders. Industrial ergonomics is the study of the work environment, the tools needed to perform the work, and how to adapt job tasks to human abilities and natural body movements. The goal of office ergonomics is to set up a workplace so that it fits an individual and the job he or she is doing, thereby alleviating stress and injury caused by awkward positions and repetitive tasks.
There would appear to be a lack of ergonomic standards, guidelines, or research specific to the design of an audiologist's work environment. A thorough review of the literature failed to produce specific results.* Representatives from the American Speech-Language-Hearing Association and Speech-Language and Audiology Canada confirmed that ergonomic information specific to the design of audiology work environments is unknown to their organizations (C. Kealey, personal communication, August 13, 2014; P. Mason, personal communication, August 13, 2014).
This case study consisted of a physical assessment of an audiologist performing a visual reinforcement audiometry (VRA) test on two clients. The participant is a female audiologist in her early 30s working with children aged 6 or under. The VRA clients are between 8 months and 2½ years of age and accompanied by a caregiver. Through interviews, observation, and a body mapping exercise, many risk factors for work-related musculoskeletal disorders (WMSDs) were identified that result from a mismatch between audiology work processes and deficiencies in the layout and design of equipment, furniture, and work area. WMSDs arise from movements, such as "bending, straightening, gripping, holding, twisting, clenching, and reaching. ...What makes them hazardous in work situations is the continual repetition, often in a forceful manner, and most of all, the speed of the movements and the lack of time for recovery between them" (Canadian Centre for Occupational Health and Safety, 2012). The audiologist engages in repetitive, unsupported, and often static muscular effort to perform her work, suggesting further awareness and research of ergonomics in audiology are needed to help define an effective "match" between audiologists, their work processes, and their environment (Pheasant & Haslegrave, 2006, p. 17).
Materials and Procedure
Observation focused on VRA testing. Wilson's (2005) "onion skin" diagram, adapted from Grey et al. (1987) is a method of organizing interactions relevant to the application of ergonomic and human factors in work design and was used to illustrate potential interacting factors affecting audiology work. The case study focused on collecting data on physical interactions among the individual, the task, equipment, and personal work space. See Appendix B for more detail.
An outline was given to the participant to explain the case study objective, the data to be collected, and the method of collection. Hard copies of a body map template (Corlett, 2005, p. 473) were given to the participant for her to document bodily discomfort throughout the course of 1 day. A questionnaire was developed to structure the interview with the participant, gather background information, and structure the observation (see Appendix A). A measuring tape, sketch pad, digital camera, and tripod were used to observe and document the work environment. The results of the body map exercise were reviewed after results from the observation had been gathered and the results from each method had been compared.
Results
Findings from the observation combined with results from the body map exercise highlight several ergonomic concerns with the work environment. In the body map exercise, the participant documented no discomfort during the morning hours, but noted medium discomfort in the neck and shoulders beginning in the early afternoon (2:30 p.m.) and at the end of the day (5:30 p.m.). These findings were similar to areas of concern noted during observing of the VRA process. VRA accounted for approximately 40% of the audiologist's workload in a working week, took approximately 45 minutes per test (although this can vary), and consisted of four subtasks: an ear examination, audiometry testing, tympanometry, and distortion product otoacoustic emission (DPOAE) testing. The audiologist used an otoscope, audiometer, headset, reinforcement box, ear probes, and tympanometer. A laptop was used for the DPOAE test. The following data were gathered from observation of two VRA tests in succession.
Subtask one: Examining child's ear and inserting ear probes, 5–10 minutes, Figure 1

Figure 1: Audiologist examines ears while standing, kneeling, and bending.
During this task, the caregiver and child sit at a table facing the observation window within the audiology booth. The audiologist examines the ear with an otoscope for ear infections, wax, or obstructions. She inserts ear probes and explains the audiometry test to the caregiver and how to distract the child during the audiometry test, using the toys in the booth, when prompted by the audiologist.
In the situations observed, the audiologist was standing, kneeling, and bending during this process. Kneeling placed her at eye level with the patient and within reach of the toy box on the floor and may have also provided variation in posture. No seat was available (presumably due to spatial constraints) and her trunk was held in a flexed position during the examination. The ear probe headset was within comfortable reach while the audiologist was standing.
Subtask two: Audiometry testing, 20–30 minutes, Figure 2

Figure 2: Less-than-ideal equipment positioning, low task lighting, and reflected glare during VRA testing.
During this task, the audiologist leaves the booth, closing a heavy door. She turns off the lights in the clinic to minimize distraction of the child using a light switch at the entrance, located far from her workstation. She sits at her desk in front of the observation window and presents a clearly audible sound using the audiometer, while simultaneously pushing a button on the reinforcement box to reveal a mechanical puppet located on a side wall within the booth. This conditions the child to look for the puppet when the child hears the sound. She uses a dial to decrease the sound in increments of 20 db until the child stops looking for the puppet, which indicates the child no longer hears the sound. She then increases the dial by 5 db increments until the child looks for the puppet. This procedure is done approximately 25 times.
In the situations observed, the participant frequently leaned back, fidgeted, and moved her feet on the foot rung of her task chair; her feet never rested flat on the floor. She held her trunk upright, rarely engaging the 300 mm high backrest. Her trunk may have been flexed to stabilize her feet and compensate for the instability from the seat height, which exceeded her popliteal height (Canadian Standards Association International, 2000, p. 174) and/or to reach the reinforcement box. Her left hand was held in extension (Pheasant, 2006, p. 147) over the audiometer's dial, and she could not rest her arm on the desk because of the audiometer's raised edge. The right hand was held in a static, extended position (Pheasant, 2006, p. 147) over the reinforcement box and was removed only to chart results on a clip board. While she was charting, her elbow was held in a static position above the work surface. The audiometer's display screen was located below the recommended 45° acceptable display zone (Pheasant, 2006, p. 169) but did not require the audiologist's attention. Task lighting was not available for charting, and daylight reflected glare in the observation window.
Subtask three: The tympanometry test, 5–10 minutes, Figure 3

Figure 3: The audiologist bending and extending while middle ear function is examined.
During this test, the audiologist measures the middle ear function of the child by inserting ear probes connected to the tympanometer.
In the situations observed, the participant's trunk was held in flexion with the neck held in extension during insertion of the ear probes and use of the tympanometer, located on a 737 mm high table. She had to extend her right arm to the far right to reach the tympanometer located behind the client. It was apparent that the work surface for the tympanometer was too low and beyond reach to allow the audiologist to maintain a neutral standing height posture (Pheasant, 2006, p. 43).
Subtask four: DPOAE test, 10–15 minutes, Figure 4

Figure 4: Additional testing requiring repeated bending and reaching.
In this task, the audiologist measures the inner ear function by inserting ear probes connected to a laptop located on a 737 mm high table. The participant continually monitors the test on the laptop for noise sensitivity. Readings from the tympanometry and DPOAE tests are printed out on an 876 mm high table located behind the tympanometer. The audiologist gives the results of the test to the caregiver.
In the situations observed, the participant's trunk was flexed with the neck extended during insertion of the ear probes and use of the laptop. Sometimes she squatted to view the laptop screen. Lights above and in front of the laptop screen were a source of reflected glare. When toys used to distract the child fell on the floor, the audiologist retrieved them. She bent over to retrieve the garbage can to dispose of the ear probes. As the parents left, the audiologist also bent over to tidy up the toys. See Figure 4.
Other work processes that exceed the scope of this study, but should be noted for their systemic relation to VRA testing, include the auditory brain stem response test (ABR), the conditioned play audiometry test (CPA), hearing aid setting, American Sign Language (ASL) consultation, data entry, and booking clients. Other interacting external factors include infection prevention and control, financial considerations, and changes in legislation. Psychological factors affecting job design could warrant further study; such factors include heavy client workloads, the challenges posed by testing children diagnosed with behavioral issues, or managing parents' frustration and despair with wait times or a troubling diagnosis.
Discussion
"Pain is the most common symptom associated with WMSDs," with early signs being "aching and tiredness of the affected limb occurring during the work shift but disappearing at night and during days off work" (Canadian Centre for Occupational Health and Safety, 2012). Findings from the body map exercise and observation suggest the audiologist may be at risk of "postural stress" and "upper limb disorders" (Pheasant, 2006, p. 105, 122, 126, 165, 177). In the body map exercise, the audiologist reported no discomfort in the morning followed by medium discomfort in the neck and shoulder area in the afternoon. Observations from the VRA procedure revealed the work environment required extensive and repetitive flexion of the trunk and neck while the audiologist was seated or bent to retrieve items from the floor; extension of the neck due to inappropriate work surface heights; excessive reach envelopes due to poor equipment layout; static extended or flexed wrist postures due to poor equipment layout and design; sustained muscle effort to support the trunk, neck, head, and elbows while seated; and visual strain and awkward postures used to compensate for dim lighting during charting and reflected glare from display screens and the observation window.
The following recommendations could improve working conditions specific to VRA. It is important to note that, without a thorough systems analysis of this task in relation to other tasks and interacting factors, it is difficult to ascertain whether these suggestions would be in conflict with other work processes or constraints.
Seating
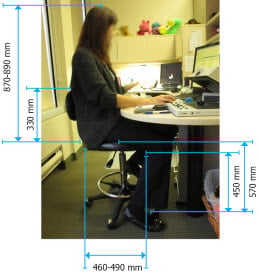
Figure 5: Optimizing the audiologist's task chair for better back and shoulder support.
Replacing the task chair should be considered, and the choice should reflect that the audiologist is "in and out" of her chair—adjusting ear probes, attending to patients, and performing other tasks, suggesting that each chair should be trialed for at least 3 hours (Pheasant, 2006, p. 122). The chair should have a seat that can be adjusted to or slightly below popliteal height (450 mm or less for this individual), a medium height back rest (500 mm) for back and shoulder support, a lockable seat angle to tilt the chair forward for detailed tasks, and adjustable lumbar support (Pheasant, 2006, p. 131-134). Padded arm rests should be evaluated with attention to desk interference (Pheasant, 2006, p. 134). Controls should be easy to use (Canadian Standards Association International, 2000, p. 174). See Figure 5.
Workstation and Equipment
Writing should be relaxed with the arm raised sideways and forwards, supported by a work surface slightly above the user's elbow height (Pheasant, 2006, p. 162). The subject's seated elbow height is approximately 690 mm–710 mm, requiring a minimum desk height of 710 mm. Padding in front of the audiometer and reinforcement box would support the forearm. See Figure 6 for suggestions on reconfiguring the workstation and equipment.
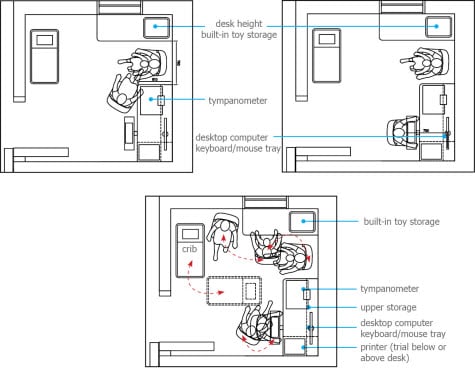
Figure 6: Suggestions for repositioning workstations and equipment.
DPOAE testing should be done while the audiologist is seated, using a desktop computer with the screen placed no farther than 750 mm from viewing to prevent extension or flexion of the neck and flexion of the trunk (Pheasant, 2006, p. 168). A keyboard and mouse tray on a surface height of 650 mm–750 mm (based on sitting elbow height) will help facilitate neutral shoulder and arm postures (Pheasant, 2006, p. 162, 168). If the task requires that the audiologist stand (due to short use or spatial constraints), then the same principles for work surface heights apply, but using standing elbow height as the basis (Pheasant, 2006, p. 33). In a revised layout, toys, accessories, and information pamphlets could be stored within reach of the audiologist, whether she is standing or sitting, to avoid flexion of the trunk. Toys could be fixed in place on a higher work surface to decrease repetitive forward bending. It is also worth questioning whether all of the subtasks need to occur in the audiology booth.
Lighting
Observers want to darken environments to study their clients but also require lighting for security, safety, or to complete tasks while observing the client (C. Corbet, personal communication, December 20, 2012). Greater flexibility and attention to layout are required to achieve some or all of the following: zone-controlled, indirect lighting on dimmers accessible from the workstation, audiology booth, and entrance area; lighting on either side of display screens to reduce reflected glare; lighting on either side of the client's face in the observation window to reduce harsh shadows caused by overhead lighting; back lighting in the audiology booth to create depth of field for observing the client; flexible task lighting where documentation is required; and the use of motorized, dual sun-control and black-out shades to control natural lighting and eliminate reflected glare (C. Corbet, personal communication, December 20, 2012).
These recommendations may be specific to this case study but are applicable to the assessment of audiology clinics in general. More detail has been provided in Appendix D. The findings suggest audiologists may be at risk of WMSDs, if the work environment does not support their work processes and anthropometry. Modifications should aim to reduce or eliminate the risk of musculoskeletal discomfort and other stressors using the closest relevant industry standards (e.g., ergonomic standards and guidelines for health care and office environments) as well as relevant building code standards. These findings demonstrate the importance of ergonomic research in audiology and challenge widely held views that "audiologists have one of the least stressful jobs" (Advance for Hearing Practice Management, 2013) and that the work is "not physically demanding" (Bureau of Labor Statistics, 2012).
*Keyword search for "ergonomics, human factors, musculoskeletal, posture, and design" produced no specifically related results in the following journals: Canadian Journal of Speech-Language Pathology and Audiology; American Journal of Audiology; American Journal of Speech-Language Pathology; Journal of Speech, Language, and Hearing Research; Human Factors: The Journal of the Human Factors and Ergonomics Society; The Ergonomics Open Journal; Canada Occupational Health and Safety Regulations; and the Canadian Standards Association Canadian Health Care Facilities Z8000-11 .
See the appendices [PDF].
About the Author
Chantal Trudel is an industrial designer consulting on health care planning and design for Parkin Architects. She is completing a master's degree in ergonomics through the University of Nottingham, has taught at Ryerson University's School of Interior Design, and is currently teaching at Carleton University's School of Industrial Design. Chantal's interest in audiology and ergonomics began while working as a staff member at Parkin Architects on the design of a children's treatment facility. The client had identified concerns with the current state of the audiologist's work environment and, through her study, Chantal discovered that audiologists' work had not been studied from a human factors perspective.
Chantal's research interests are focused on ergonomics and health care design. She has worked on large, multi-disciplinary project teams, including the Health Sciences Centre (HSC) Women and Newborn Hospital in Winnipeg, Manitoba, and the McGill University Health Network P3 Competition in Montreal, Quebec. Chantal's work has also been featured in Canadian Interiors for the design of McClelland and Stewart's head office, when she worked for B+H Architects. With Parkin Architects, she has received the Canadian Architect Award of Excellence in 2010 and a High Commendation from the International Academy for Design and Health in the International Future Health Project Category 2012 for the HSC Women and Newborn Hospital. Contact her at chantal@aneurin.com.
References
Bureau of Labor Statistics. (2012). U.S. Department of Labor, Occupational outlook handbook, 2012–13 Edition, Audiologists. Retrieved January 04, 2013, from http://www.bls.gov/ooh/healthcare/audiologists.htm.
Canadian Centre for Occupational Health and Safety. (2012). Work-related musculoskeletal disorders (WMSDs). Retrieved January 1, 2013 from http://www.ccohs.ca/oshanswers/diseases/rmirsi.html.
Canadian Standards Association International. (2000). Guideline on office ergonomics Z412-00. Toronto, Ontario, Canada: CSA International.
CareerCast. (2014). The least stressful jobs of 2014. Retrieved August 14, 2014, from http://www.careercast.com/jobs-rated/least-stressful-jobs-2014.
Corlett, N. E. (2005). Static muscle loading and the evaluation of posture. In J. R. Wilson & N. E. Corlett (Eds.), Evaluation of human work. Boca Raton, FL: CRC Press Taylor & Francis Group.
Health and Safety Executive. (2003). Work with display screen equipment. Kew, Richmond, Surrey: HSE Books.
Pheasant, S. & Haslegrave, M. (2006). Bodyspace. Boca Raton, FL: CRC Press Taylor & Francis Group.
Wilson, J.R. (2005). Methods in the understanding of human factors. In J. R. Wilson & N. E. Corlett (Eds.), Evaluation of human work. Boca Raton, FL: CRC Press Taylor & Francis Group.










